Cardiologist on call
Flying Doctor Telehealth makes it easy to prioritise your heart health.

When it comes to heart health, Dr Anthony Dortimer is adamant that prevention is better than a cure.
“If people know how to live sensibly and healthfully, we can prevent a considerable amount of heart disease,” he says. “I think that’s been well-shown through the treatment of cholesterol and blood pressure, by not smoking, managing weight and exercising. All of those things are likely to dramatically diminish the likelihood of getting heart disease.”
Dr Dortimer has been a practising cardiologist since 1980. He has worked in various practices and hospitals across Victoria, including the Austin Hospital, and is currently the military cardiologist in Victoria. He is also a member of some prestigious worldwide societies, including the International Andreas Gruentzig Interventional Society, which is dedicated to research, publication, study and teaching in the fields of cardiovascular disease.
Additionally, Dr Dortimer is a part of RFDS Victoria’s Telehealth team, having joined the program in 2017 due to a desire to help people in rural communities.
“In my experience, rural patients perhaps may not be quite as aware of preventative health treatments as city patients, and maybe that’s because there aren’t as many doctors out there,” he says.
This sentiment is echoed in a research paper RFDS published last year entitled, 'Equitable Patient Access to Primary Health Care in Australia'. In this paper, we found that many of the severe COVID-19 patients internationally were reported to have an underlying history of hypertension, diabetes, coronary heart disease, COPD and renal disease. As remote populations have both higher rates of these conditions and poorer access to primary health care and preventative services, they are particularly vulnerable should COVID-19 infection rates increase in these areas.
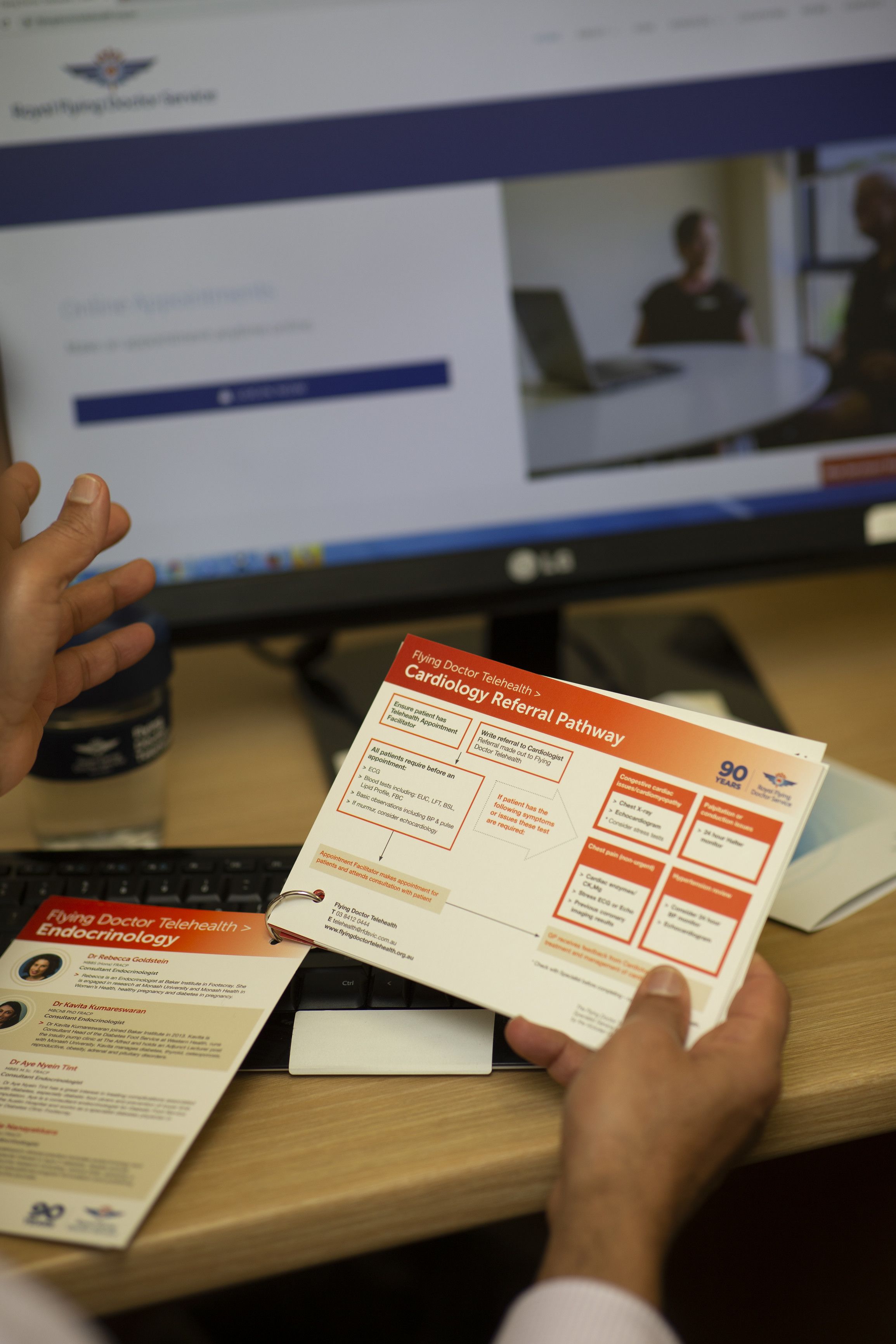
What Flying Doctor Telehealth does is attempt to bridge this geographical gap between rural communities and health care specialists. In doing so, Telehealth helps to negate the factors that typically see people from rural communities find it challenging to prioritise their health.
Consider this: you live in a remote Victorian community some 400km from your heart specialist in Melbourne. Your doctor has recommended that you come into the city every three months for important tests, but in order to stick to this schedule, you need to take a day off work, drive four and a half hours each way and pay for a tank of petrol and parking – and then do it all again in a few months’ time. It’s easy to understand how maintaining these appointments can feel too hard for some people, and how rural communities can be critically disadvantaged by distance.
With Flying Doctor Telehealth, patients need only visit their GP or local health centre to connect with specialists like Dr Dortimer via a phone or video call.
“Telehealth is a really helpful thing. I can look at a patient’s results, listen to them and then tell their GP what tests should be done,” says Dr Dortimer. “I think Telehealth has a significant role to play; it’s quick and convenient and I think patients get a lot out of it.
“I think it has a future and we’ve proven already in the past few years that it’s been beneficial. And the doctors who have used it have tended to come back to us. So I think they think it’s helpful for their patients.”
When it comes to staying on top of their heart health, Dr Dortimer recommends people in rural communities remain vigilant and proactive about common symptoms.
“Shortness of breath, chest pain, palpitations, swelling of the legs – they’re all reasons to seek advice,” he says. “People have to listen to their body. They have to be aware of what’s going on with their body, and if they find something different, go to their GP. And then if there is any question, they need to get a heart check as well, and that’s where we come in.”
A GP can provide a referral to Dr Dortimer via Flying Doctor Telehealth, allowing any suspected problems to be escalated quickly to a specialist. “If the GP says, ‘we can provide you with Telehealth with the Flying Doctor cardiologist almost immediately’, that has to be a good thing.”
However, because many health issues related to the heart have no symptoms, like an irregular pulse or high blood pressure, it’s critical that everyone over the age of 60 commit to an annual check-up, even if they think they are symptom free.
During an annual check-up, Dr Dortimer recommends that patients insist on having their bloods done and ensuring their doctor listens to their heart, takes their blood pressure and measures their pulse. “Surprisingly, GPs don’t always do that, and I always say to my patients, you need to demand from your GP to do those things, not just accept that they don’t do them.”
In terms of heart health, people in their 60s and 70s need to be particularly vigilant of risk factors and symptoms, as they are the most prone to heart disease. “It seems if you get through your 60s and 70s, quite often you’re then well for your 80s and 90s,” says Dr Dortimer.
Dr Dortimer allows 45 minutes for each of his Telehealth appointments, with a patient’s GP encouraged to sit in on the call too. “I then have time on that consultation to talk about risk factors and try and educate the patient as well.”
Flying Doctor Telehealth is available for a range of specialist appointments, not just cardiology. Our team currently includes medical professionals from eight specialist fields, all of whom can be reached via a GP referral. Visit the Flying Doctor Telehealth website for up-to-date information on all of our available specialists.
By negating the need to travel long distances to see a specialist, a Telehealth consultation can save money and time. And if accessibility is the difference between someone prioritising or neglecting their health, Flying Doctor Telehealth could also save a life.